How ketamine infusion therapy works, what it feels like, and what it’s used for.
Emily Pisacreta // April 21, 2021
DoubleBlind Mag is devoted to fair, rigorous reporting by leading experts and journalists in the field of psychedelics. Read more about our editorial process and fact-checking here. Editorially reviewed by Madison Margolin.

Ketamine Infusion
If ketamine could talk, it would have a lot of stories to tell. Since it was developed in the 1960’s, ketamine has been used as an anesthetic on wounded soldiers on the battlefield, for children and adults in hospitals, and for pets being treated at the vet. It’s on the World Health Organization’s list of Essential Medicines. It’s been an underground favorite of partygoers at raves and concerts. Now, for the last several years, the medical community has been tapping into ketamine’s potential to treat psychiatric conditions. In particular, ketamine has demonstrated powerful and rapid reversal of suicidal thinking in a majority of patients who undergo ketamine infusion for depression.
Ketamine treatments, including esketamine nasal spray, ketamine infusion therapy, and other ketamine formations are now being used to fight not only for depression, but other psychiatric disorders like anxiety, PTSD, OCD, substance use disorders, and even non-psychiatric conditions involving chronic pain. There are multiple ways ketamine can be introduced into the body—including lozenges, injections, or nasal spray. Here’s everything you need to know about one of the most popular methods, and the one most subject to clinical study: ketamine IV infusion.
Ketamine IV Infusion: How Does Ketamine Infusion Therapy Work?
Ketamine treatment has generated a lot of excitement in the field of psychiatry as it’s one of the first new treatment options for depression in almost half a century—and its effects are lightning fast when compared to existing treatments. With many common antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) or monoamine oxidase inhibitors (MAOIs), relief from depression and suicidal ideation can take up to several weeks. With ketamine IV infusion, clinical studies have shown suicidal ideation and depression symptoms can begin to reverse within a few days, or in some cases, even within hours of beginning treatment.
What does ketamine do in the brain to cause such a miraculous turn-around? Like other psychiatric medications, the exact mechanism of action is not 100 percent known. But scientists do have an idea of what ketamine gets up to in the brain. One major theory is that ketamine binds to NMDA (N-methyl-d-aspartate) receptors, which can have powerful downstream effects, activating the production of BDNF (brain derived neurotrophic factor), growing and strengthening connections that were offline before. Dr. Lori Calabrese, a psychiatrist who treats patients with ketamine infusion at her clinic in South Windsor, CT, compares BDNF to a kind of fertilizer for the brain’s dendritic branches, which are stalled in those suffering from depression.
“In the brains of people whose stressors turn on this incredible overdrive response with inflammation, the production of that fertilizer BDNF drops way down, and the structures become really, really pruned,” she says. “We think that what ketamine can do is enhance re-arborization of those trees, and it can do it quickly.”
What is Ketamine Treatment Like?
While ketamine infusion for depression has been investigated for almost 20 years, it’s still in many ways an emerging field. The only ketamine-related treatment for depression that is currently approved by the FDA is a prescription nasal spray known as esketamine, marketed under the brand name Spravato. When doctors and other health care providers administer ketamine infusion for psychiatric conditions like depression, anxiety, or PTSD, it’s considered an “off-label” use of the drug. The process of receiving a ketamine infusion can vary depending on where you go.
Ketamine IV infusion is available at many outpatient treatment facilities in many different states, from independent clinics to major research hospitals. Ketamine infusion therapy usually involves a series of treatments delivered over the course of a few weeks. You’ll work with a health care provider throughout the process of receiving ketamine treatment, though the kind of provider may vary depending on what kind of ketamine clinic you go to. According to the American Society of Ketamine Physicians, Psychotherapists & Practitioners (ASKP3), the majority of ketamine clinics are operated by anesthesiologists, certified registered nurse anesthetists (CRNAs), psychiatrists, and advanced practice mental health professionals.
There are differing views among various medical fields about what kind of provider is best suited to the provision of ketamine therapies. In the Journal of Psychedelic Psychiatry’s recently published “Ethical Guidelines for Ketamine Clinicians,” the authors suggest that the ketamine clinics provide two essential roles: a mental health professional and a medical health professional. A psychiatrist is a provider who can fill both roles. In the case of clinics run by anesthesiologists, emergency doctors, or nurse anesthetists, a mental health provider like a psychotherapist or licensed social worker should also be involved in patient care, according to the guidelines.
Dr. Steven Mandel is an anesthesiologist by training who has spent the last seven years providing ketamine infusion therapy at the Ketamine Clinics of Los Angeles in Culver City, CA. He agrees that caution is warranted when it comes to selecting a ketamine infusion provider. He recommends looking at credentials and experience, and avoiding anyone who seems to be overpromising or overselling.
“It’s not a cure,” he says. “It’s a treatment, and it’s not a standalone treatment. It’s a treatment that is enhanced enormously when applied in conjunction with other treatments.”

One important thing to look out for is whether the provider takes the time to get to know your medical or psychiatric history before offering treatment, he says. At Dr. Mandel’s clinic, that means consulting with other physicians or therapists before allowing a patient to embark on a course of ketamine infusion whenever possible.
For Dr. Calabrese in Connecticut, it means first sitting down with potential patients for 60-90 minutes, in an attempt to really get to know the patient, their medical and psychiatric treatment history, and their goals for ketamine therapy.
“It’s really important for me to get an idea of what someone used to be like the last time they were in a good place for at least a good year,” she says. She will also try to consult with a patient’s primary care physician or psychiatrist if they’re already seeing one.
The overall process for receiving ketamine infusions can vary from place to place, but the basic steps of ketamine infusion will usually go something like this:
- You’ll contact a clinic, answer screening questions, and schedule an appointment
- You’ll meet with the provider and/or a psychiatrist, psychologist, or social worker to talk about your medical and treatment history to find out if ketamine infusion may be right for you
- You may have a physical screening to check for things like high blood pressure
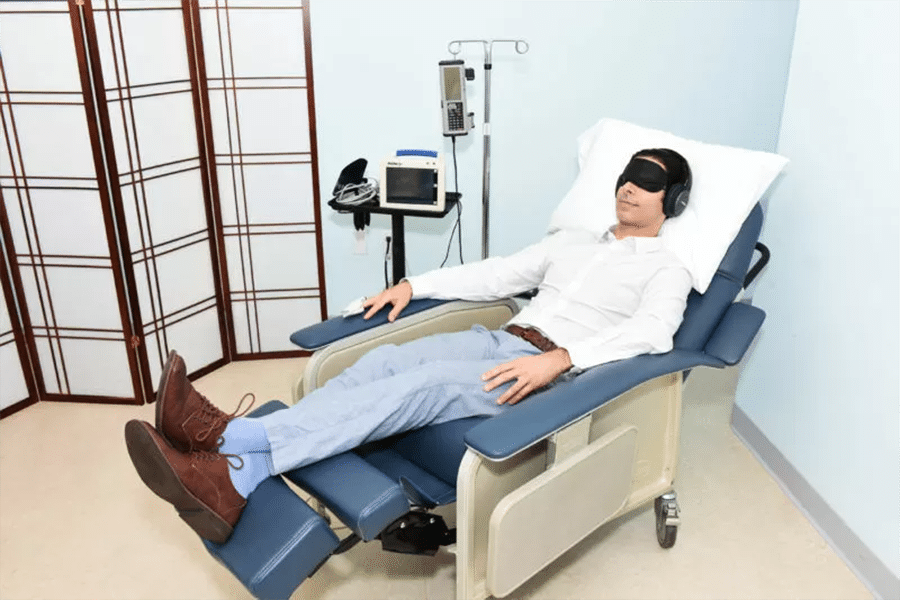
- You’ll receive an intravenous infusion of ketamine and saline solution for about 45 minutes
- You’ll schedule subsequent infusions (usually two or three a week for a period of two to three weeks) and receive follow up care as needed
In the days after your ketamine treatment, your provider may want to spend time talking with you about your experience during the treatment—a process known as integration. Integration helps you make sense of the experience and apply it to your life outside of the clinic.
Ketamine Infusion: Experience and Side Effects
So, what does ketamine infusion feel like? In order to experience the therapeutic benefits, what’s required is a dosage of ketamine strong enough to induce a temporary dissociative state but not strong enough to fully sedate you. That dissociative state has been described as a dream-like, out-of-body, and even holy experience by some patients. For most people, it’s an overall pleasant and calm feeling, but for some it can feel disorienting or anxiety-provoking. A very small number of patients experience a level of distress during ketamine infusion that makes them want to stop the treatment.
Dr. Calabrese tells her patients that they can expect to feel extremely relaxed in the beginning of the infusion, and may experience some numbness or tingling in their fingers, toes, and lips. After some time, the experience evolves, moving from a daydream-like state into what is known as a “non-ordinary state of consciousness.” Some patients even experience fleeting visual, auditory, and olfactory distortions during their infusion.
It can “feel almost like your thinking, or your mind and heart, are really outside of your body—almost as if you’re floating in the universe,” she says, “or almost as if you are open to messages that the universe wants to give you.”
During that time, your ketamine provider or staff at the ketamine clinic will likely monitor your blood pressure, pulse, and oxygen, and check in with you about how you’re feeling. After the infusion, the dissociative effects take about 15-20 minutes to completely fade away. At the end of your session, you can expect to feel a little dizzy and likely very tired. Most providers will require that you have a ride home from the ketamine clinic, and advise you not to drive or operate any heavy machinery for the next 12 hours. You may not feel fully back to normal until after a good night’s sleep, which is why many providers offer ketamine infusions in the late afternoons and evenings.
The side effects of ketamine IV infusion are minimal. In a survey that asked ketamine providers to report adverse events, the most commonly cited side effect that resulted in patients discontinuing ketamine infusions were feelings of distress, happening in about 0.5 percent of patients. All other side effects occurred in less than one percent of patients.
Most ketamine treatments are relatively short-term, encompassing only a few weeks of treatment. But the potential side effects of longer term use of ketamine are less clear. Long term abuse of ketamine outside of the clinical setting is associated with painful urinary tract problems and cognitive impairment.
Ketamine Infusion: Dose
Ketamine infusion dosage depends on what you’re using ketamine infusion to treat. Based on much of the literature published on ketamine for depression and mood disorder, the American Psychiatric Association recommends a dose of 0.5 milligrams per kilogram of the patient’s body weight over the course of 40-45 minutes.
However, depending on the provider, the ketamine infusion dose may vary slightly from patient to patient, or even from infusion to infusion. In Dr. Mandel’s practice, he adjusts the dosage as he monitors his patients. His method involves checking his patients’ eyes for certain movements that indicate whether the patient is receiving a dose that will deliver the intended relief. For many of his patients, that can mean a slightly higher dose at certain points in their treatment than that standard 0.5 milligram per kilogram.
“There’s a sweet spot, and the sweet spot is pretty narrow,” he says. “The sweet spot [also] changes with the patient’s experience with the drug.”
Ketamine Infusion for Depression
The first placebo-controlled, double-blinded trial of ketamine infusion for depression was published in 2000 by researchers from Yale, and the results were pretty blockbuster. Pre-clinical research had suggested that the neurotransmitter glutamate might have something to offer in terms of treating depression, and they wanted to try using an NMDA receptor antagonist—ketamine—in patients with depression. In the seven patients treated with ketamine infusions, all had a marked reduction in depression symptoms.
Since then, several randomized, double-blind studies have provided further evidence that ketamine infusion provides what the American Psychiatric Association calls “rapid and robust, albeit transient” treatment for depression. In the organization’s list of recommendations for ketamine therapy, the literature they cite as most reliable suggests a success rate of about 70 percent for reversing depression symptoms.
Ketamine is also proving to be notably effective at rapidly reducing suicidal thinking. Dr. Calabrese is the author of one such study. Published in the International Journal of Psychiatry, the study is a review of findings from treating 231 adults and adolescents in her clinic that showed a decrease in suicidal thinking in 79 percent of the patients. A randomized clinical trial published in the American Journal of Psychiatry showed a greater reduction in clinically significant suicidal ideation in patients treated with ketamine infusions than those treated with another sedative.
Ketamine Infusion for PTSD, Anxiety, OCD, Substance Use Disorder, and Other Mood Disorders
Treatment resistant depression has been the most closely studied mental health condition when it comes to ketamine infusion. However, there are studies that show ketamine’s potential to treat a variety of other mood disorders, including generalized anxiety disorder, post-traumatic stress disorder, obsessive compulsive disorder, social anxiety disorder, postpartum depression, and even substance use disorder. Ketamine clinics regularly offer treatments for these conditions—which frequently coexist with depression—in much the same fashion as ketamine infusion for depression.
Ketamine infusion for PTSD shows particular promise, with a number of small randomized clinical trials showing a rapid and significant reduction in PTSD symptoms when compared with those treated with another sedative, midazolam.
Similarly designed studies by Dr. Elias Dakwar and other researchers at Columbia University comparing patients treated with ketamine infusion to midazolam showed promise treating substance use disorders, including alcohol use disorder and cocaine use disorder.
Dr. Calabrese says many patients show up at her clinic concerned that they won’t be eligible for ketamine treatment because of their substance use disorder. But she says the evidence that ketamine treatment can help people with substance use disorder is striking.
“I’ve used it in the office to help patients as they’re tapering down on Suboxone, as they’re struggling to not relapse on opioids after they’ve had rapid opioid detox under anesthesia, and as they’re struggling with cocaine.”
Even though ketamine infusion for mood disorders and substance use disorders show a lot of promise, ketamine is still not considered 100 percent effective at treating anything. Some patients don’t respond, and research hasn’t established why.
Ketamine Infusion for Pain
One major area of growth in the world of ketamine is its use as a treatment for chronic pain. Clinics are offering ketamine for pain related to fibromyalgia, neuropathy, complex regional pain syndrome (CRPS), migraines, and more.
In general, researchers note that more high quality research into chronic pain and ketamine is badly needed. However, existing research is promising. One meta-analysis from 2019 revealed that pain relief benefits continued on past infusions for up to two weeks in many patients receiving IV ketamine. In a 2017 review of protocols for treating neuropathic pain with ketamine infusions, the authors were able to conclude that the duration of relief from neuropathic pain was associated with longer, higher dose infusions, and that the addition of sedative medications such as midazolam or clonidine helped patients avoid unwanted psychotropic effects. Still, the authors noted that the literature needed to create a comprehensive set of recommendations for effective dosing is lacking.
Ketamine Infusion Cost
Ketamine infusion, unless it’s used as an anesthetic or analgesic (pain reliever), is considered an “off-label” use of ketamine. That means that ketamine has not been approved for sale by the FDA for the purpose of treating mood disorders, chronic pain, or anything other than a narrow set of uses in clinical settings. While it’s perfectly legal and very common for doctors to prescribe a drug or treatment off-label—it doesn’t necessarily mean it’s unsafe or doesn’t work. Unfortunately, it can make insurance companies less likely to cover it. While some insurance providers are starting to come around to covering ketamine infusions, it’s often the case that patients have to pay out of pocket. Still, it may be worth checking with your insurance provider about coverage and reimbursement—especially if your insurance covers one provider in your area but not another.
Without insurance, ketamine infusion cost can range from $350 to $1000 per infusion session, according to a report in STAT that reviewed dozens of clinics across the country. A typical course of treatment with ketamine infusions involves two to three infusions per week for a period of two to three weeks—up to nine infusions total. That can be a financial strain for many people who may benefit from ketamine. As such, some clinics offer payment plans or take credit cards, and some may even offer treatment on a sliding scale.
Is Ketamine Therapy Right for Me?
Ultimately, the best way to know if ketamine therapy is right for you is to talk with an experienced ketamine provider as well as your current doctor, psychiatrist, or therapist. If you’re dealing with depression, anxiety, PTSD, chronic pain, or substance use disorder, ketamine may be worth a look—especially if you haven’t responded to other, more standard treatments. But it’s important to note that ketamine infusion therapy is definitely not for everyone. In general, it may not be right for people with the following conditions:
- Untreated high blood pressure
- Untreated thyroid disease
- Unstable heart disease
- Current manic phase of bipolar disorder
- Current psychosis or history of psychosis
While ketamine infusion may be a treatment option for some people with depression associated with bipolar disorder, those who take lamotrigine may not be good candidates for ketamine infusion according to Dr. Calabrese. Lamotrigine can make ketamine less effective and may complicate the treatment process. She has also found in her clinic that people who use a lot of cannabis and who don’t want to ramp down their use before ketamine treatment generally don’t respond as well—a phenomenon that she believes needs more study.

It’s important for your ketamine provider to know what medication you already take and what conditions you are currently and have in the past been treated for. For that reason, both Dr. Calabrese and Dr. Mandel recommend finding a provider who will work in conjunction with other health care providers you may already be seeing, like your psychiatrist, primary care physician, or any other doctor who prescribes you medicine.
If you’re feeling depressed, it’s incredibly important to get help. This is especially true if you’re having thoughts of suicide. Even if ketamine therapy isn’t the answer for you, talking with a licensed mental health professional, or even opening up to someone close to you, can make a huge difference.
I every day wish I had the opportunity to try this treatment. Than k you Barbarabearden15 @.com I always I don’t want anything just peace. Which I work hard at and I’m 60/40❤️