
Time magazine recently offered a Special Edition on mental health… Did you see it?
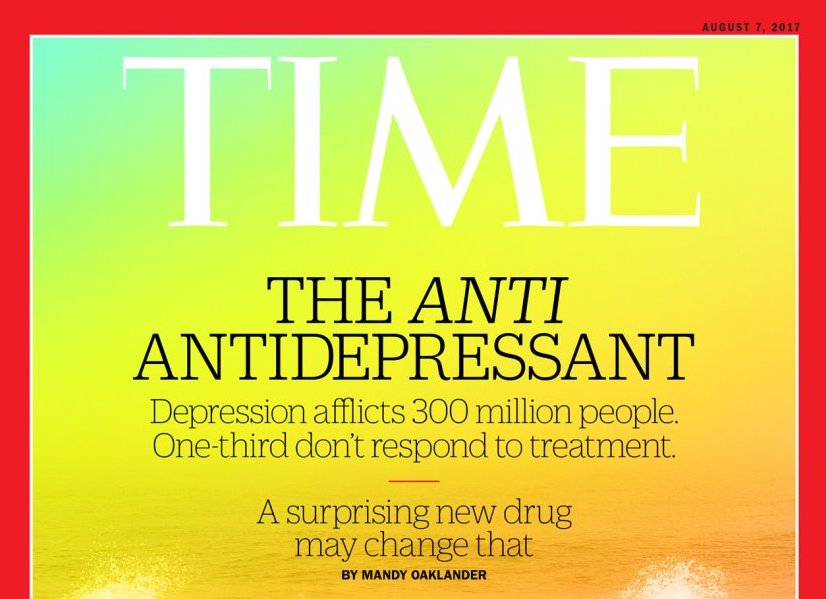
The article about depression treatment – and ketamine specifically – by Mandy Oaklander published in July 2017, was reprinted for this special edition. The title of the special edition is “A New Understanding”…but since the article Oaklander wrote is two years old, I’m concerned this special edition may be misleading.
Her cover article two years ago touted ketamine as an “anti-antidepressant.” This same term is repeated on this Special Edition cover. But, since Oaklander’s article created some misunderstanding when it was first printed, I’m not sure it’s accurate to refer to the contents of this edition as “a new understanding.”
In fact, some of her representations of ketamine treatment border on archaic.
Ketamine and Depression Treatment
The field of ketamine for depression treatment is a new field in the “psychiatry and neuroscience universe” that’s been growing at break-neck speed. A wide variety of healthcare professionals offer this treatment in a wide variety of places and using a wide variety of methods.

Still, because we’re on this quest together, you and me, I want to take a few minutes to express my perspective on this reprint of her article.
What quest?
Well, that would be our passion to find more ways more people can be relieved of the symptoms that impair their lives.
We talked about this after this article was published in TIME two years ago. But we’ve learned so much since then. Through neuroscience research as well as in private psychiatry practice and in meeting and collaborating with other healthcare professionals at national and international conferences since then.
What Have We Learned Since TIME Published That Cover Story?
Lots. About ways to prolong the effects of ketamine, ways to prolong and maintain remission, more of the actions of ketamine in the brain… We focus on ketamine treatment. So let’s talk again now about how she framed ketamine treatment in a less accurate light than we might wish.
Because if you suffer, you want to know. You try treatments and medications for months – and years – in vain. You want to know that you’re getting the best possible information you can get your hands on.
Regarding the route of administration
This article spoke of a lady named Barbara Reiger who’d been depressed since childhood. It said that since no other treatment helped, she goes monthly to a ketamine clinic. And there she has “a needle full of ketamine plunged into her deltoid…”
This route of administration for ketamine treatment is only one of many. In the 2 years since the article, there has been much more research about IV ketamine infusions. The intramuscular route is less predictable than an IV for getting the medicine on board. In addition, it’s more difficult to manage the onset of action or the experience once ketamine is sealed into muscle. You can’t slow its absorption or effects, or stop it.
We later read that Ian Hanley, another person with treatment resistant depression, received ketamine infusions. I assume these are intravenous (or IV). The term “infusion” speaks of the IV route. (Though surprisingly, I hear there are those who use this term to refer to IM injections. This isn’t correct, and can be so misleading to patients who don’t know the implications.)
Is Ketamine and Depression Treatment a “Trip?”
Another point is the experience itself: Is it a “trip?” What does the patient experience with ketamine treatment? Oaklander calls these treatment experiences “ketamine trips” as though the concept of a psychedelic trip is the foregone conclusion with ketamine treatment. While it’s true that there will be a variety of experiences between various patients, and that ketamine is a visionary medicine, ketamine treatment for depression should not be confused with people who use ketamine for a psychedelic trip.
Oaklander’s perspective focuses on ketamine as a psychedelic drug. Such characterization draws a narrow crowd of people interested in psychedelic exploration, but can alienate the larger population of patients who have no interest in psychedelic anything. It’s a misunderstanding of ketamine and its properties to limit the characterization of it.
Who’s in Charge? The Medicine or the Doctor?

And it’s the responsibility of the physician administering the medicine to use a route, a rate, and a dose that allows the patient to know the ketamine is actively working. And to prepare and protect the patient from an overwhelming experience.
As it takes action in (1) her brain circuits, (2) her BDNF to proliferate synapse connections, (3) her lateral habenula, and (4) those G proteins on lipid rafts in the cell membrane, the patient will experience sensations, feelings, and possibly visuals as a result. (Amazing, isn’t it? These are just a few areas of action we know about ketamine! There may be far more!)
Because the brain is made up of nerves that connect with each other, and complex systems that perform vital functions of all types, impacting these circuits gives you certain sensations, thoughts, and experiences.
The sensations feel overwhelming if the dose is too high. And the patient can feel alarm if the rate is too fast or uncontrolled. In fact, the experience might even advance to something you might call a “trip.”
But … a closely monitored infusion should prevent the overwhelm, while allowing full restorative freedom for the medicine to do its work.
Ketamine Can Erase Suicidal Thoughts in an Afternoon

Oaklander also pointed out the rapid and dramatic ability of ketamine to stop suicidal thoughts in a few hours, whether it relieves depression or not.
This is a shining benefit of ketamine — that its ability to erase suicidal thinking is separate from its antidepressant benefits. Lifesaving.
Now about how ketamine lifts depression. Oaklander wrote that the “ketamine trips,” as she called them, help people disconnect from their bodies and thoughts. Her idea was that this experience changes the mindset so completely that the depression lifts.
However, while we know the experience is important as part of the ketamine and depression treatment, research presented at the American Psychiatric Association Conference in San Francisco a couple weeks ago shows it’s not enough to lift the depression by itself. In addition, if that were true, those who have had these “trips” would all be depression–free … and that’s not true either.
Even so, the dissociation the patient experiences during the infusion does serve as a sign of what’s actually going on in the brain. This is ketamine at work, restoring synapses, turbo boosting BDNF. This process is not for entertainment but rather it signals the restorative properties at work, just as pain signals something wrong in the body.
How Ketamine Works… There’s More to Learn
Oaklander’s statement that “experts aren’t sure exactly how ketamine works…” is still true, but we know far more than we did when she wrote the article two years ago. It seems this one medicine has spawned its own frontier, and we keep learning. Research on ketamine for psychiatric disorders presses on around the world.
And real-world practices also present data to give the medical community, and our patients more information that ketamine has taught us.
Learning more about what we already know is paramount. A recent study revealed how ketamine restores brain circuits. We understood that it did… or believed that to be so. But now a two-step process in restoring dendrites and dendritic spines has been revealed through a special laboratory process. This is the tip of the iceberg.
There is so much more we want to know about this extraordinary treatment.
Ketamine and Depression Treatment in General: Keep the Research Coming
And this is where I’d like to see journalists like Mandy Oaklander and her contemporaries use their influence to call for more research. It’s wonderful that pharmaceutical companies continue to search for new possibilities in drugs to target more areas of the brain. The more the better.

But, as Oaklander pointed out in that article, the concern and caution about ketamine lies partly in its potential for abuse, but also in its potential for damaging side effects.
Our concern is that it may be damaging eventually if it’s used too often for too long.
For those who receive ketamine infusions every few weeks or every single month with no end in sight, there may be risks. Since ketamine can help such a large population of people with treatment resistant disorders achieve resilience and remission… isn’t it worthy of the research to find out more that it can do? To build our body of knowledge…?
How many more people can be restored with ketamine infusions if we find out what their physiological and psychological obstacles are? What do we need to learn to remove more of the hindrances to an individual achieving resilience… and even remission?
It’s true that not everyone responds to ketamine treatment. We’ve talked about how preliminary research suggests that those with the VAL-VAL allele respond so quickly, and those with MET-MET can respond more slowly, or sometimes not at all.
But there are also those who respond within the first three infusions, but then their response dissipates. These are responders, and yet not remitters. There are studies that suggest differential responses in certain groups, like the Taiwanese. Let’s find out what we don’t know about why.

In some cases, there’s a cerebral folate deficiency that hasn’t been treated, in others it’s Low T, in others it may be deficiencies only found in the cerebral spinal fluid…
And if deficiencies that cause depression are there, they need to be teased out and treated, so ketamine can do more to restore those lives.
But..what other obstacles are there that can be treated so our patient can get the most out of his ketamine infusions…and enjoy resilience… and get the most out of his life?
We applaud all efforts to find more treatments that will be effective for more patients. But rather than focus on ketamine’s potential danger in the long term, why not invest our resources in finding out how to get more people to remission so they’re NOT exposed for the long term?
What if that pot of gold at the end of the rainbow is not in fact another medication we also don’t fully understand, but rather a better understanding of the one that works so well already?
Thank you, Mandy Oaklander of TIME magazine, for spreading the word about this new frontier in treatment two years ago. While your characterization seemed to stray from our perspective through neuroscience, we have appreciated that TIME magazine helped to make this breakthrough treatment a household word. We’re learning so much and the more we learn, the more we see that we NEED to learn.
Knowledge really is power against psychiatric symptoms.

Here’s hoping we can all walk together to get effective treatment to more people. Several years ago, studies showed that “60-70% of people with treatment resistant depression respond to ketamine” … but we’re making progress.
A number of doctors in private practice are learning to get more out of each infusion for better outcomes for our patients. And we’re seeing responses much higher than 60-70%.
At Innovative Psychiatry, we see extraordinary outcomes in our patients every week. Patients who were too ill to work, who had withdrawn from their relationships, and lost hope in their jobs, their lives, and themselves…go forward to find initiative, resilience, joy, and bushels of hope for a fulfilling and rewarding life after they receive carefully supervised ketamine treatment.
If you suffer and endure with symptoms of depression, PTSD, bipolar depression, addiction, social anxiety, and suicidal thoughts... give yourself the opportunity to feel better and live better. Call us and find out what joy feels like.
