I just returned from the annual meeting of the American Psychiatric Association’s Institute for Psychiatric Services: Mental Health Services Conference, in NYC.
This conference was presented in collaboration with the World Psychiatric Association. The World Psychiatric Association represents 120,000 psychiatrists in 120 countries. The heart and focus was that innovation and collaboration improve access to psychiatric care. It’s easy to miss the numerous populations who struggle to get help. And need it so desperately.
What a wonderful gathering. This group convened for psychiatrists and all the allied professionals who work together in mental health. Social workers, therapists, psychologists, counselors, psychiatric nurses, and mental health workers on every level. With the theme, “Improving Access Through Innovation and Collaboration,” the sense of learning and sharing together was palpable.

An audible commitment pervaded the crowd who recognized not only the value, but the vital role each discipline plays to provide mental health care to those who need it. The President’s theme concept definitely found its mark. Innovation and collaboration improve access to psychiatric care for everyone.
Abundant Presentations
There were presentations about suicide, about issues for LGBTQ youth, about the mental health and well-being of physicians and medical students, about addiction, and about where opioid use and psychiatric disorders intersect. There was a round table discussion about the presence and needs of mental health sufferers in the criminal justice system, an area sorely in need of solutions.
One session informed about talking, and listening, to patients about marijuana and CBD, and provided information psychiatrists need to know for these discussions.
Poster Presentations on 3 Floors
Then there were poster presentations. Four separate sessions of them!
Poster presentations on the latest findings in a wide variety of current subjects. One presented the issues that come into play when a patient requests a hastened death. Heavy subject matter, without question. Another considered a case of delusions of persecution in someone suffering from migraine. Another reported on psychiatric needs in the refugee crisis. Still another described educating an underserved community about ADHD.
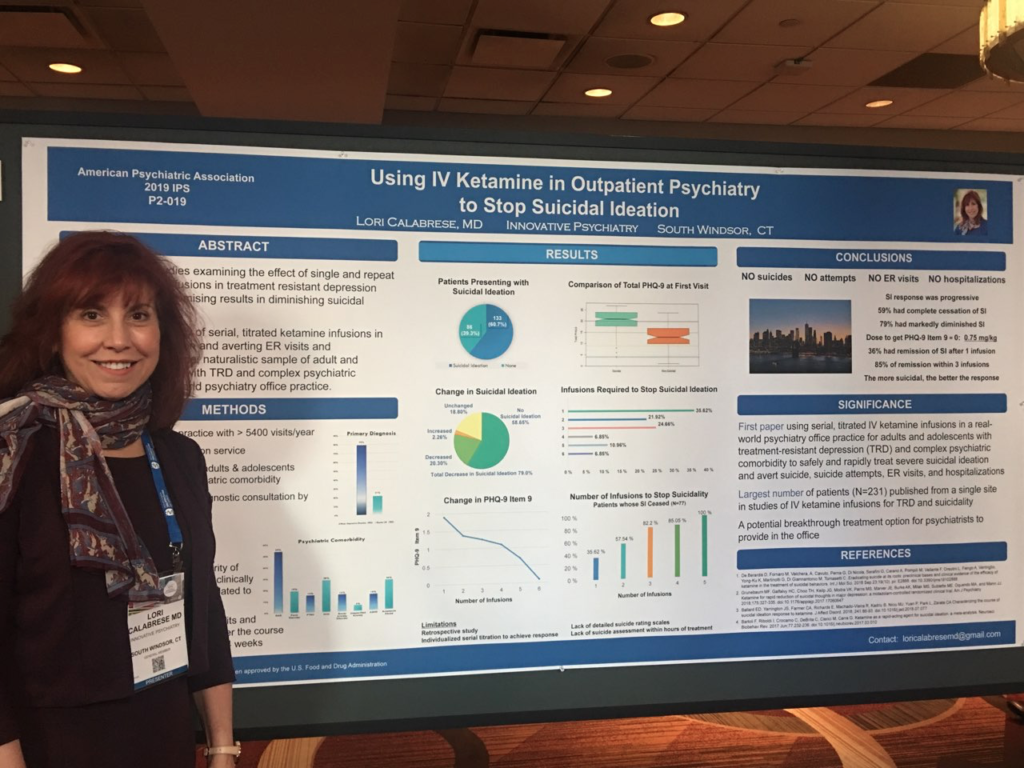
And there were several on suicidality, where I also presented my own findings in treating suicidal thinking with IV ketamine infusions.
The enthusiasm for my poster bubbled over. So many asking questions, wanting discussion and details. I wish I had had more time. But it was thrilling to see how much psychiatrists ache to have better treatment alternatives for their most vulnerable patients. I think many were captivated by the fact that out of this population we had no suicides, no suicide attempts — not even trips to the ER. No one needed to be hospitalized.
IV Ketamine Treatment Can Make Such a Difference
IV ketamine treatment really is a game changer. And it can be a life-saver. We’re learning — and have so much more to learn— about how infusion dose and dissociation play a huge role in the outcomes.

We read the literature. (It keeps us up at night!) And we trust the literature. And sometimes we allow the literature to even think for us… So it really helps when our colleagues try an approach we haven’t heard of especially if it turns out to be effective. It adds a tool to our tool belt.
When we go to conferences, one of the driving forces is that we’re always hoping to find another tool or two we can use to help our patients improve.
It was thrilling to me to talk with other psychiatrists who would like to learn more about how ketamine can help, and who want to make sure they know enough about it in real practice settings to begin to talk with their patients about if, when, and how much. We all want better tools, better responses, better results. We need to be careful, thoughtful. And bold enough to stay on the cutting edge.
Some were hand-picked by the President of APA
There were presidential presentations, which were arranged by Bruce Schwartz, M.D., President of the APA. He invited specific leaders to speak on pressing subject matter from their expertise and experience.
One highlight was the presidential presentation by the esteemed Charles Nemeroff, M.D., Ph.D. He’s Professor and Associate Chair for Research at the University of Texas Dell Medical School in Austin, TX. Dr. Nemeroff has published more than 1100 scientific reports focused on the pathophysiology of mood and anxiety, particularly in children of abuse and neglect.
Dr. Nemeroff’s presentation centered on personalized medicine in psychiatry. His point of view is that personalized medicine is advancing slowly, but as we move forward, the future for our patients shines brighter and brighter.
I see the importance of his words in my own practice, and with my own patients. There is always room for improvement. Now, more than ever, the stakes are high, and time is short.
The Tragedy of Inmates Who Need Treatment

Another presidential presentation that was deeply felt by many was a round table discussion. It was chaired by Althea Jeanne Stewart, M.D., regarding the disjoint between mental health needs and the criminal justice system.
If you’ve ever encountered the experience of an inmate with a disordered brain, you know— the pain and frustration these suffer, the frustration of staff, and the intense difficulties for everyone involved.
We must continue to confront these difficulties in our system, and do the hard work required to apply better solutions.
Innovation and Collaboration Improve Access to Care for All Patients

The theme for this year’s conference was a solid one. Ongoing innovation will yield more effective treatment. And in collaborating with a team of experts, more psychiatric patients will have the care they need. But one of the stakeholders is the insurance industry and the insurance companies who pay for care. We need them to realize that and innovative treatment like IV ketamine can stop suicidal thinking enough to reduce their dollar spend on ambulances, mobile crisis calls, ER visits for suicidal ideation and hospitalizations for people who fear they will harm themselves.
Because as we advance forward, our society will only benefit from a broader and larger population of people who are functioning well, and feeling well. Who can fill their positions, contribute their talent, raise their children, take care of their world. For that to happen requires accessible psychiatric care.
And in the case of outpatient care in the privacy of an office setting, extraordinary treatments like IV ketamine …could mean the difference between life and death.
We see it every week at Innovative Psychiatry. Not only life and death struggles, but life that’s rewarding. Full of hope. Where purpose, meaning, and reward replace despair. Where you have the energy and creativity to restore and strengthen your relationships. And where joy thrives.
We attend meetings to bring home more to help you find restoration. If you have severe symptoms of depression, bipolar depression, social anxiety, PTSD, substance use disorder, or postpartum disorder, call us. We’ll help you find out if IV ketamine treatment can help you heal and find joy and purpose in your life.

To the healing of your best self,
