
Like other disorders of the brain and mind, bipolar disorder is complicated.
With all the movies and cartoons made at the expense of people who suffer from disorders like this, we want to help more people know more about some of the facts with a bit of bipolar science.
It’s different for each person. The length and intensity of manic episodes, the distribution of time from one end of the spectrum to the other. How hallucinations and delusions fit into the mix. These symptoms are individual.
It’s physical. It can shake and shatter your body, through intense and sudden swings from one extreme to another.
Plus, it can cause such unexpected assaults on your emotions that your body is exhausted. Those swings can feel almost like a convulsion at times.
It can also create sensations. Some people with this disorder complain of feeling like they have fire ants on their brain. Of course, there are no insects involved. But the disordered circuitry creates a sensation in some cases.
And it’s mental. It changes your perceptions of what you see and hear. By coloring the way you interpret what happens, it tattoos that impression deeply in your memory. It can distort your view of yourself, and marinate your thoughts in shame. Then it can turn on the firehose of pain and rage, until you’ve experienced such extremity of horror, you can feel like you sweat blood.
But, that’s not all. Bipolar disorder also seems spiritual, sometimes pulling you into its dungeons of horror until you lose all connection to your own spirit. Righteous indignation can morph to revenge. A little anxiety can billow until it’s a life-threatening terror.
And yet, this disorder can be all of these things, or it can be none of them. OR… you can begin with these experiences, then medication can help them melt away. OR… there may be no medication that mitigates them at all.
What you can’t know when all that is happening, is that specific changes in your brain cells are translated to the violent swings and misery you face in your daily life. You may find yourself craving a bit of bipolar science to try to gain perspective about what’s happening to you.

To help reduce the stigma surrounding bipolar disorder, and the behaviors of people who suffer so deeply from it, let’s look at a tidbit of breakthrough science related to the spectrum of “bipolar disorders.”
A Bit of Bipolar Science…
You’ve heard of the blood-brain barrier, right? Relatively few people outside the medical field have any remote idea what that is. So if you’ve heard of it, consider yourself “in the know.” Kudos!
OK. There are two types of blood barriers in the brain. One is the blood-brain barrier, or BBB. The other is the blood-CSF barrier. And that’s the one we’re going to talk about now.
So the blood-CSF barrier keeps the blood and whatever is in it separate from your cerebral spinal fluid (CSF). Since the CSF is constantly washing the brain tissues, it needs to be free of contaminants, toxins, or components that are harmful to the brain’s delicate circuitry and structures.
The CSF performs a couple of primary functions. One is to cushion and protect that most vital organ – your brain – that keeps everything else humming along. And the other is to keep the toxins in your brain and spinal cord flushed out.
CSF and the Choriod Plexus
But…Where does the CSF come from?
So glad you asked. The choroid plexus produces this most vital and beneficial fluid. There are special cells that secrete it, and other tissues absorb it.
Because the ventricles of your brain can handle 150ml of CSF at a time, but the choroid plexus actually makes 450ml a day! Clearly, as it circulates, it also is absorbed or drained off and replaced by more.
This keeps your brain cushioned and protected by fresh CSF at all times.
If the choroid plexus makes too much CSF, and if the pathway for draining off excess become blocked, then the amount of CSF in the brain can increase dangerously, increasing pressure in the brain. And a condition known as hydrocephalus can develop, along with the risk of brain damage.
By the same token, if the choroid plexus makes too little CSF, the brain cannot function. And the cushion it provides to help it remain buoyant within the bony chamber of the skull is inadequate.
So there’s a need for balance between the CSF, the cavities in the brain, and the circulation of it.
About Psychosis
So let’s talk about how the choroid plexus relates to schizophrenia and bipolar disorder with a bit of bipolar science.

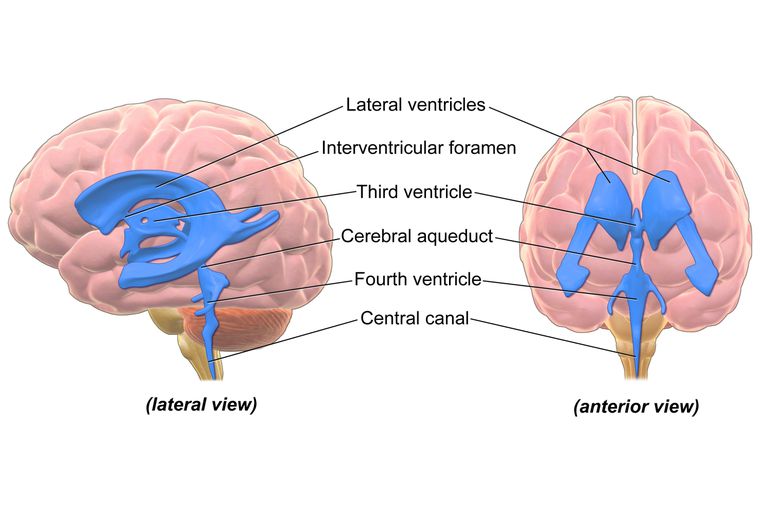
There are four cavities in the middle of the brain called the ventricles. The CSF washes and cushions the brain all around, and is produced and distributed from choroid plexuses in these ventricles.
New Research
Newly published research sponsored by Brain and Behavior Research Foundation (BRRF) has directly linked the size of the ventricles with psychosis. While the size of ventricles is not specifically correlated to schizophrenia and bipolar disorder, the volume of the choroid plexus is significantly larger in subjects with psychosis.
In addition, these researchers found that the volume of the choroid plexus in siblings, parents, and children of those with psychosis was less than the affected individual but still significantly larger than those unaffected by psychosis in their family. This demonstrated that the volume of the choroid plexus is something one inherits to a large degree.
But here’s the big news.
They found that when a subject had a larger choroid plexus, they also tended to have lower cognition, less grey matter, a smaller amygdala, larger ventricles, and fewer connections between neurons.
All of these things can be connected to the pathological processes that cause psychosis.
Now that’s news.
But there’s more.
That increased size in the choroid plexus in subjects with psychosis was also associated with increased levels of interleukin 6 (IL-6). IL-6 is a signaling cell in the immune system.
So here’s the rub.

IL-6 can penetrate and seep through the protective barriers between the brain, blood, and CSF. Since researchers know that IL-6 is a strong suspect connected to bipolar disorder and schizophrenia, the identity of the gang of thieves behind psychosis – you might say – seems to be emerging. Add to that the connection between IL-6 and the reduced amount of grey matter in the cerebral cortex, and the case just grows stronger.
“Our findings suggest the involvement of the choroid plexus across the psychosis spectrum, with a potential mechanism involving the neuro-immune system, which functions in regulating the brain and interacting with the body’s immune and inflammatory systems,” the team concluded.
If you struggle with bipolar disorder, schizophrenia, or episodes of psychosis, you may appreciate the work of these researchers that sheds more light on what happens in the brain causing these difficult episodes.
Neuroscience researchers are making great strides in learning more than has ever been known before about the symptoms of these disorders. And the more we understand, combined with a bit of bipolar science, the more research will lead to better treatments.
No matter what your difficulty, whether you struggle with bipolar disorder, PTSD, social anxiety, severe depression, or even thoughts of suicide, we may be able to help. IV ketamine treatment is emerging as a dramatic game changer for people who suffer from specific types of symptoms. And happily, the types of symptoms keep growing in number.

But if you think you’d like to know if IV ketamine treatment might help you, please call us. We’ll help you find out if you might be a candidate for ketamine…because some people aren’t. But if ketamine is for you, you can experience a transformation in your own life.
While ketamine isn’t showing promise for psychosis, it can bring remarkable relief to your depression symptoms. Every little bit helps, doesn’t it?
Since bipolar depression can be the most debilitating symptom for many patients, resolving the depression in your illness can make your life so much more manageable.
As research learns more, we’ll be right there using it to help our patients. Our whole purpose is a better life, and more hope, for you.

To the restoration of your best self,

Lori Calabrese, M.D.