“I hope I don’t have bipolar disorder.”
“It’s not bipolar, right?”
“How do I know if it’s his bipolar disorder or if he’s just being a brat?”
“Everyone just throws that term around like it’s the menu of the day—bipolar disorder is so overdiagnosed, it’s not funny.”
The words are tough to hear. The phrases can feel ugly.
And the diagnosis often carries fear and even shame for a lot of people who feel judged, scrutinized, and stigmatized by it.
But the fact is, bipolar disorder is caused by changes and variations in your brain and how it works …with all its sparks and fire, and all its awful, slow sludge. Changes you couldn’t possibly have prevented. You aren’t to blame. And we’re here to offer you the support and treatment you need.
So, let’s chat a bit about what those physical causes are. We know that bipolar disorder causes extreme changes in mood, behaviors, and thinking. Your mood changes can happen over a period of months, or weeks, or even hours.
You may feel happy and energetic. Or you might feel extremely stimulated with feelings of creativity, power, and superiority for a few months. Or…intensely irritable, volatile, and impatient. It can change on a dime.
This can last for hours, or days on end, or for months.
Then your feelings can change…slowly or more abruptly… to a dark melancholy or despairing depression for just as long. Or maybe shorter. Or maybe longer…Yikes.
Not Easy. But Also Amazing…
Bipolar disorder is not fun. It’s tough, it’s exhausting, and it can dig you into a hole fast. Still, there are aspects of this disorder that can actually be amazing. Things like a perception of beauty, and heightened creativity, and exquisite sensitivity that can give you a much more delicious taste of life than the average guy on the street.
People who find their mood is dark and melancholy for months, then finally begins to brighten for awhile, experience the most common form of bipolar disorder.
But you know what? Just as the changes may happen over a long period of time, they also may swing over a period of weeks, days, or hours, with happy or agitated periods of energy, then crashing to a pit of despair, then back again… even in the same day.
The frequency, the intensity, the breadth of the symptoms – and the rate of switching – vary widely across the spectrum of the disorder.
Meanwhile, it’s important if you have these mood swings over either a short time frame, or a much longer period, that you take the step to get a thorough evaluation. If your moods and your behaviors change in a way that makes you feel out of control of your life, or like you’re sort of trapped in your emotions, then that’s your signal to reach out for an evaluation. You don’t have to figure it out all alone.
Because we’ve been working on figuring it out for centuries.
Circular Insanity
Sounds pretty awful. You may know that a generation ago it was known as manic depression. And before that, in 1851, it was called circular insanity. The condition we now call bipolar disorder reaches back to the earliest observations of despair and melancholy in 400 BC. It’s not new. It goes way back. Misery has always been easy to spot.
But early psychiatrists, who were attentive and meticulous observers, recognized that in some people, despair had another face in bipolar disorder. A person could suffer from one illness that had two extremes, rather than two separate conditions. And…the two extreme symptoms were related to each other.
Medicine has researched bipolar disorder deeply since that time, and it is the most fascinating and possibly the most broadly researched and investigated brain-based health condition.
That’s right. Bipolar is not just bad behavior, or uncontrollable anger, or a flaw in someone who doesn’t control himself. It’s a brain-based condition that needs treatment.
The National Institutes of Health says that 2 percent of Americans suffer from this disorder. But of that 2 percent, they say 83 percent are particularly severe.
Other surveys put the numbers much higher when you take a broader perspective and include more subtle forms of depression and mania—at anywhere from 3 to 10 percent.
So Many Without Treatment Struggle … And Feel Misunderstood
Here’s the tragedy, though. Because of the stigma sometimes associated with this diagnosis, as well as misidentification of the symptoms, misunderstandings about the treatments, and financial constraints, not even 40 percent are treated with even minimally adequate treatment.
That means there’s a huge number of people struggling every day in their work, their relationships, and their homes, unable to understand why everything is so hard. Why they feel so alone and misunderstood.
Sometimes a person with bipolar disorder feels like he or she’s actually got two different sides: the “wild” one who stirs up problems …. and the “nice” one who has to live with the fallout.
And that’s what treatment is about — to create stability, to help the “wild” one blend into the nice one so life, work, and relationships are manageable again.
But What About You?
What does this mean for you and your family?
One thing we know is that there’s a tendency to inherit this disorder. So if you see these symptoms in yourself or your child, someone else nearby in the family tree very likely has it, whether they’ve been diagnosed or not.
If you aren’t the one in your family with bipolar disorder, you may wonder what your role is and how to cope with the ups and downs. Keep reading … we’re going to address relationships with a person who has bipolar disorder in future posts.
Hopefully, this post will help you gain some understanding of what your loved one goes through, and why.
Bipolar disorder, like other brain-based disorders, is not a sign of weakness or bad behavior in the person who has it, but rather is a result of changes in the structure and function of certain anatomic elements of the brain.
The Amygdala in Bipolar Disorder
One key area that’s a source of symptoms for this disorder is the amygdala, which is located in the temporal portion of the brain. This little lima bean-shaped duo organ is located on each side of the brain, in the temporal lobes. The amygdala alerts us to fear, it responds to things that are rewarding, and is also the seat of aggression. It identifies for us those things in our environment that are emotionally important to us.
If a fire is ignited near us, we see danger. In a bipolar person that alarm is multiplied. If we see something rewarding, like a bar of chocolate, or a fragrant flower, or the sweet smile of a baby, the amygdala lights up, and we feel a flush of pleasure.
But if you have bipolar disorder, the response of the amygdala is exaggerated and you may feel that reward with far more intensity.
Basically, the amygdala activates far more emotion in persons with bipolar disorder than it does in the rest of us.
So you feel those emotional reactions with more intensity.
And understandably, you’re likely to express those emotions with more intensity, too.
There’s also evidence that the amygdala itself is smaller in children with bipolar disorder, and is assumed to be too small; but it’s been reported as both smaller than it should be… or larger in adults with this disorder. There’s still so much to learn.
Let’s look, though, at more of the brain structures that explain still more about bipolar disorder.
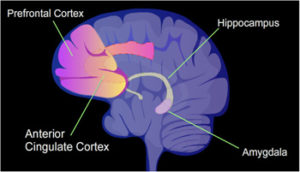 The Prefrontal Cortex – Dorsolateral and Ventral
The Prefrontal Cortex – Dorsolateral and Ventral
Another key area in the brain that’s significant for you if you have bipolar disorder is the prefrontal cortex. It helps us consider facts and choose our behavior in response. This area helps with mood regulation, and helps us inhibit behaviors we may feel like doing, but know are not socially advantageous to display.
There are two key players in the prefrontal cortex for people with this bipolar disorder. They’re the dorsolateral prefrontal cortex, and the ventral prefrontal cortex.
The ventral prefrontal cortex is securely connected to the amygdala. Like the amygdala, it also responds to what’s rewarding or not rewarding. In people with bipolar disorder, it responds with more intensity than it does in those who don’t have this disorder.
The dorsolateral prefrontal cortex is the more rational part, and tends to moderate emotional reactions. In people with bipolar disorder, it’s far too inactive.
Which means that the emotional networks of the brain in bipolar disorder are exceptionally active, and the networks that moderate those emotions are less active or ineffective.
The result? Highly active emotions in a person who doesn’t have the equipment to regulate them. Plus highly stimulated aggression, again without the inhibitions to control it. This is a brain that just can’t do its job.
Bipolar Disorder is a Biologic Illness
All of this is to say that bipolar disorder isn’t an excuse for misbehavior–as sometimes cruel, uninformed individuals might think. It’s the result of altered areas of the brain that heighten emotion when that brain is also lacking the equipment it needs to manage emotional responses.
For this reason, if you live with bipolar disorder, you can know this is a condition just as real as diabetes or heart disease and just as debilitating.
And just like other illnesses, if you have bipolar disorder or other mood disorders, you need support and help through treatment.
We’ll talk more soon about how this disorder affects your life, your work, and your social connections. But for now, let’s just understand that your illness is caused by things in your body that aren’t working properly. Those things need to be treated.
Some people experience a stable and rewarding life with the right medicine, good therapy, and good structure in their lives. But some need an alternative treatment to enjoy a fulfilling life.
Experience Improvement
The only way to determine what might be most helpful for you as an individual requires a thorough evaluation with diagnostic tests.
That’s why we’re here. We have the expertise it takes to tease apart complex symptoms from the complex life stories that embed them, to rule out other conditions that mimic or masquerade as mood disorders, and to offer sophisticated solutions to get your mood, thinking, and behavior back on track.
And we offer an array of treatment options to help you find your best self — including effective ways to stimulate the firing of large neural networks with TMS, and ground-breaking opportunities to stimulate your own neuronal rearborization with IV ketamine.
There have never been more exciting opportunities to get well and stay well.
Call for an appointment so we can do a full evaluation, and create a plan for you.
You can experience a more fulfilling and rewarding life, even with a diagnosis like bipolar disorder. You just can’t do it alone.
Contact me and let’s get started.
In support of your best self,
Lori Calabrese, M.D.


Dr. Calabrese, you really made having Bipolar Disorder make sense in this article. I’m going to print it and give it to everyone who I love. Thank you.